OptiThyDose: Intelligent Digital Decision Support Tool to Personalise Dosing for Children with Thyroid Diseases
Hypo-/hyperthyroidism manifests at birth or during childhood. Prompt and adequate medical treatment is key to protecting cognitive and physiological development in affected children. Dose optimisation is complex as there is a wide spectrum of thyroid disease severity and activity, developmental pharmacology, and inter-individual variability in drug kinetics and response in these children. As such, there is frequent over- and under-dosing despite international treatment guidelines. This project aims to develop an intelligent decision support tool “OptiThyDose” that computes and optimises personalised dosing for children afflicted with a thyroid disease. The researchers will use international multi-centre studies to validate and facilitate the clinical use of OptiThyDose in different socio-economic settings.
Thyroid hormones are critical for normal brain development, growth, and puberty. Hypo-/hyperthyroidism manifests at birth or during childhood. Thus, prompt, adequate medical treatment is crucial to protect cognitive and physiological development in affected children. Current guidelines recommend standard dosing regimens, despite a wide spectrum of disease variability in terms of severity, activity and receptivity. Over- and under-dosing is frequent, making a decision support tool for optimal and fine-tuned personalised dosing essential for adequate medical care.
The aim of this project is to provide personalised treatment plans for children with a thyroid disease. The consortium will build upon their existing work on an intelligent decision support tool that optimises and computes personalised treatment dosing. The researchers will use computer models that consider individual disease characteristics obtained from observational studies in combination with optimal dosing algorithms to develop an intelligent clinical decision support tool “OptiThyDose” to personalise and optimize dosing regimens. OptiThyDose iteratively computes individual dose regimens based on the patient's age, weight and disease severity to restore and maintain thyroid hormone balance.
The consortium will conduct a multi-centre study across four countries in order to validate it as a simple, robust and affordable clinical support tool in a variety of healthcare systems, including low- and middle-income countries. This individualised dosing strategy aspires to meet the needs of children with hyper- or hypothyroidism, enhance their health outcomes and support their families and caregivers independent of socio-economic status.
Banner image above: OptiThyDose is a computer programme that optimises treatment of hypo-/hyperthyroidism in children.
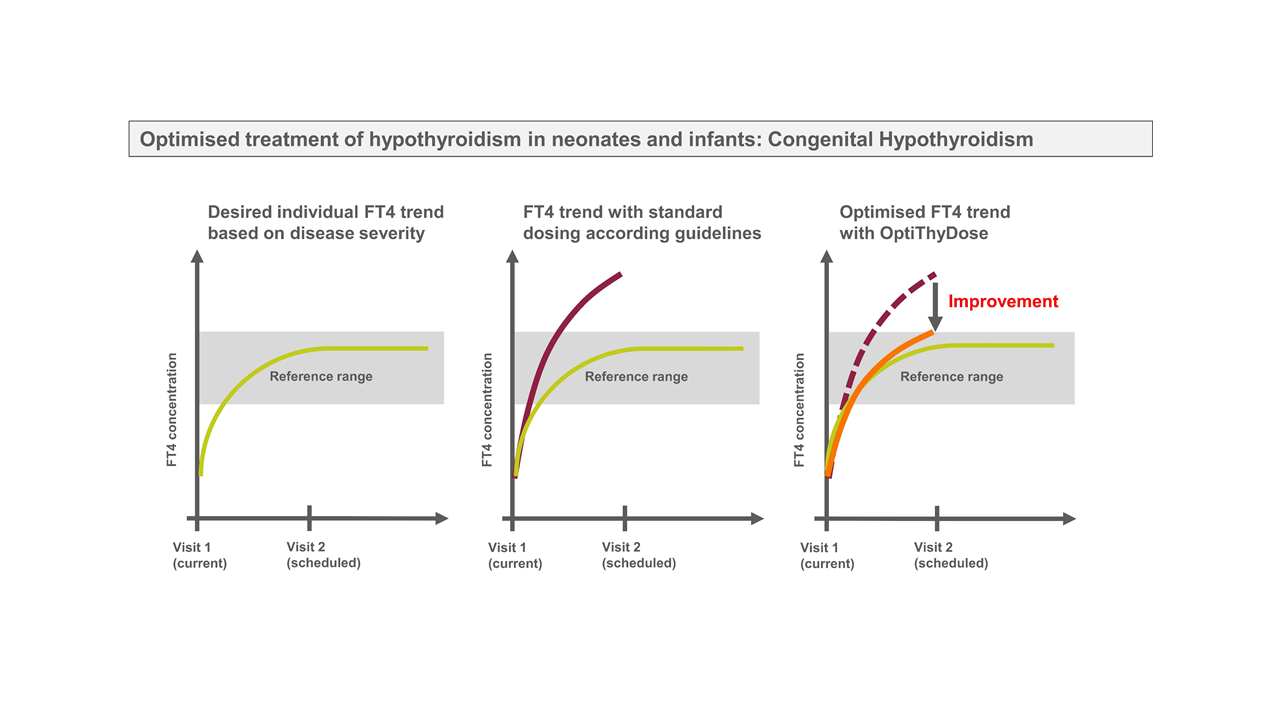
OptiThyDose is a computer programme that optimises treatment to improve individual FT4 response in children with hypothyroidism. FT4 is the main hormone produced by the thyroid and used as a biomarker used to monitor thyroid function. Image: Gilbert Koch, Marc Pfister, Gabor Szinnai
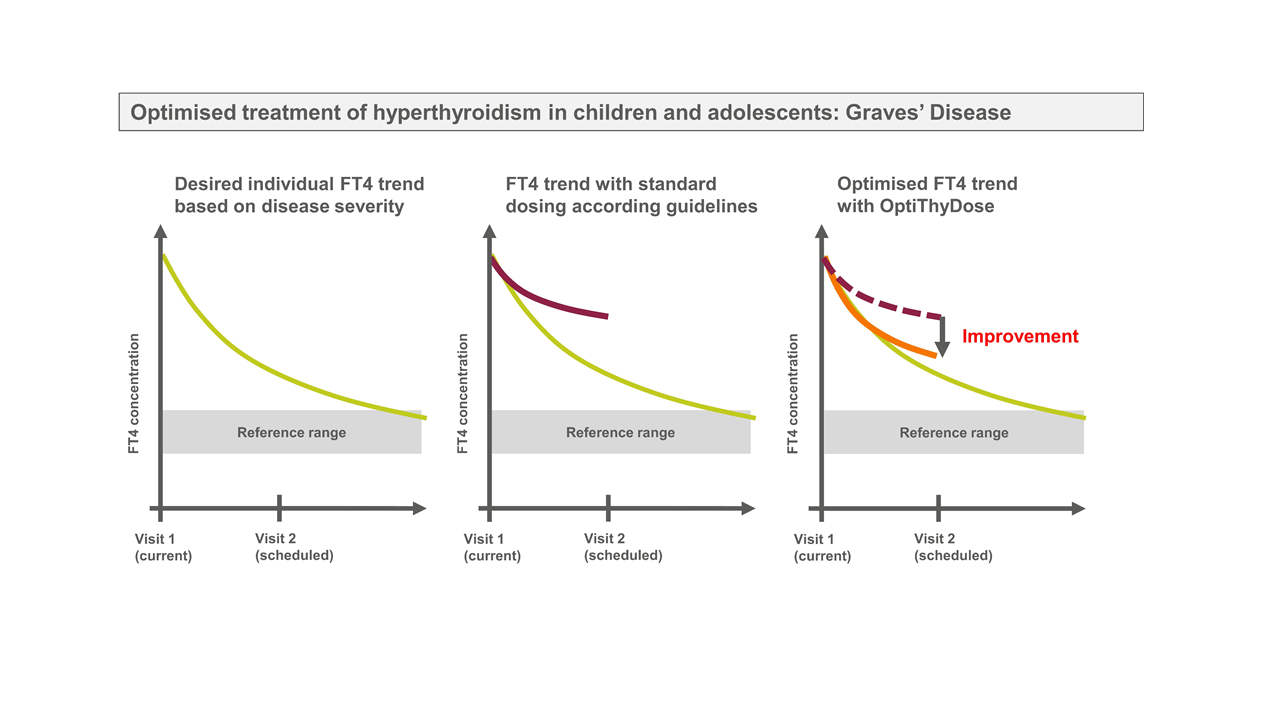
OptiThyDose is a computer programme that optimises treatment to improve individual FT4 response in children with hyperthyroidism. FT4 is the main hormone produced by the thyroid and used as a biomarker used to monitor thyroid function. Image: Gilbert Koch, Marc Pfister, Gabor Szinnai
Additional Information
- The research is part of the BRCCH Principal Investigator Initiative.
- The consortium is led by investigators Prof Gabor Szinnai and Prof Marc Pfister.
- Additional team members include Prof Marco Cappa, Prof Lusine Navasardyan, Prof Michel Polak, Prof Johannes Schropp, Freya Bachmann, Dr Fabian Claude, Dr Ricarda Foulk, Dr Gilbert Koch, Dr Laura Paone, and Britta Steffens.