January 30th 2023
A New Approach to Understand Patients’ Incomplete Recovery from COVID-19
In a study* published in the journal Nature Immunology, Prof Christoph Hess (University of Basel and University of Cambridge, UK), Dr Hélène Ruffieux (University of Cambridge, UK), Dr Glenn R Bantug (University of Basel) and international collaborators present a new approach to understand incomplete recovery from SARS-CoV-2, including long COVID, based on biological features such as cellular and metabolic changes.
Why do people react so differently to the SARS-CoV-2 virus, especially in the long term? How does the course of the immune response after infection relate to clinical sequelae i.e., the chronic effects following the disease’s initial acute phase? A team from the Cambridge Institute of Therapeutic Immunology and Infectious Diseases followed a group of 215 patients between late March 2020 and early August 2021 to study the dynamics of recovery from SARS-CoV-2 infection and the biology underlying patient-to-patient differences. The study cohort covered a spectrum of clinical severities: from hospitalized and ventilated patients, to patients with only mild or no symptoms. Uninfected healthy individuals also participated in the study, serving as controls.
A patient-centric study design
"We were primarily interested in collecting biological data, not at the level of the virus, but at the level of the host, i.e., the patients", says Prof Hess, senior author of the study. Specifically, the team wanted to investigate differences in cellular immunology, in inflammatory proteins and in metabolism over time at the patient level. “The goal of our work was to define the biological features characterizing patients with unfavourable outcomes, irrespective of demographic or clinical information”, explains Prof Hess.
To evaluate how biological parameters encompass information about the extent and dynamics of recovery from infection, the research team deployed a statistical framework tailored to the longitudinal analysis of multiple related parameters. This allowed them to reconstruct the disease trajectories of individual patients, and to characterize differences in their immune and metabolic profiles over weeks to several months post infection. Based on parameters measured soon after disease onset, they then built a predictive model and thus identified an early biological signature, predictive of poor prognosis.
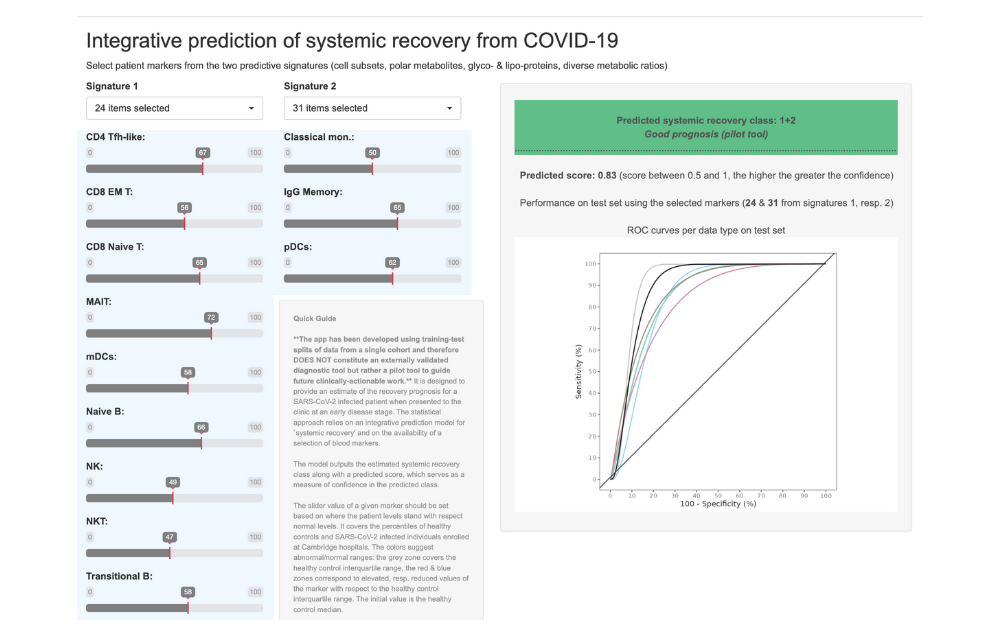
New predictions based on the biological signature can be generated using their online tool (pictured above), designed to test the research findings prospectively. Not (yet) meant for clinical use! Image courtesy of Ruffieux et al. 2023
Explore the tool yourself at http://shiny.mrc-bsu.cam.ac.uk/apps/covid-19-systemic-recovery-prediction-app/
The biological markers of long COVID
So which biological parameters are we talking about? Prof Hess explains:
- There is – unsurprisingly – the aspect of inflammation: High and persistent inflammation correlated with long-term sequelae. In particular, the levels and dynamics of the C-reactive protein, an indicator of inflammation in the body, during the acute and convalescence phases were associated with the overall recovery profile of patients, months after infection.
- The researchers also found strong predictive value of a measurement of a type of innate immune cells, the natural killer (NK) cells. Specifically, low NK cell numbers were associated with poor outcomes. How exactly NK cells contribute to the pathophysiology of SARS-CoV-2 remains to be defined.
- Interlinked with the immune response, tryptophan metabolism has been implicated in the pathophysiology of long COVID. Tryptophan (an amino acid) is a precursor of the neurotransmitter serotonin, which regulates mood and other key bodily functions. However, tryptophan can also be funnelled into the kynurenine pathway. During inflammation, such as triggered by SARS-CoV-2 infection, this breakdown pathway is induced, diverting tryptophan away from the one leading to the formation of serotonin.
Indeed, Prof Hess, Dr Ruffieux and their team did discover low serotonin levels in a subset of the patients they studied. At the same time, they found an accumulation of potentially neurotoxic metabolites, which are formed as degradation products of the tryptophan-degrading metabolic pathway.
All this, says Prof Hess, coincides with one important clinical aspect of long COVID: "Key clinical elements of long COVID can be that patients experience a lack of concentration, patients tire quickly, and they may show signs and symptoms of depression. This fits with the excessive activation of the kynurenine pathway."
Clinical relevance
Prof Hess and his newly founded start-up company, Hornet Therapeutics, identified a drugable metabolic target that may affect serotonin levels, and aim to perform a clinical trial in patients with long COVID. If preventing depletion of serotonin indeed is effective to ameliorate the above-described symptoms, this would constitute a major step in the treatment of long COVID.
Background
Prof Christoph Hess leads the Immunobiology lab at the University of Basel and is the Professor of Experimental Medicine at the University of Cambridge, UK. Prof Hess’ research focuses on the translational aspects of lymphocyte function and its metabolic basis. The goal of his work is to improve our understanding of patients suffering from disorders of immunometabolic regulation.
Read more about the BRCCH-supported research of Prof Hess and co-author Dr Glenn R Bantug- ISINC-19: Immune Senescence in COVID-19. This project is part of the BRCCH’s Fast Track Call for COVID-19 Research.
Interview article: Irène Dietschi
*Research Paper
Hélène Ruffieux, Aimee L Hanson, Samantha Lodge, Nathan G Lawler, Luke Whiley, Nicola Gray, Tui H Nolan, Laura Bergamaschi, Federica Mescia, Lorinda Turner, Aloka de Sa, Victoria S Pelly, The Cambridge Institute of Therapeutic Immunology and Infectious Disease-National Institute of Health Research (CITIID-NIHR) BioResource COVID-19 Collaboration, Prasanti Kotagiri, Nathalie Kingston, John R Bradley, Elaine Holmes, Julien Wist, Jeremy K Nicholson, Paul A Lyons, Kenneth GC Smith, Sylvia Richardson , Glenn R Bantug , Christoph Hess. 2023. A patient-centric modelling framework captures recovery from SARS-CoV-2 infection. Nature Immunology. https://www.nature.com/articles/s41590-022-01380-2